Common Causes of Vertigo and Imbalance:
Vestibular Neuritis
Dizziness and vertigo are common presentations to the Emergency Department, and some will have vestibular neuritis. The only symptom is acute vertigo, usually accompanied by nausea/vomiting. There may have been a brief prior episode hours or days before the main attack. Unlike a brainstem stroke vestibular neuritis patients can usually walk, albeit with difficulty, and prefer to lie down away from the symptomatic side.
The cause is thought to be reactivation of the herpes simplex virus in the vestibular nerves.
Diagnosis
The main clinical sign is a brisk horizontal-rotatory nystagmus beating away from the affected ear, with unsteadiness on walking. There must be a positive head impulse test confirming a reduced or absent vestibulo-ocular reflex (VOR) on the symptomatic side. A normal head impulse test should raise the suspicion of a brainstem or cerebellar stroke and the need for an MRI scan of the brain.
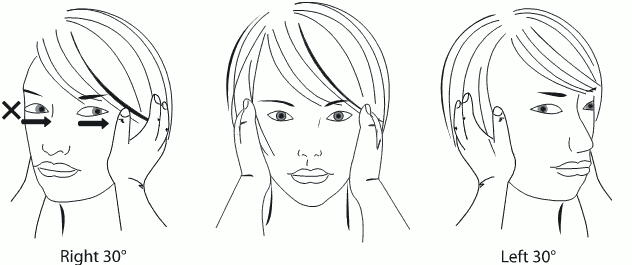
Head impluse test: This is to test the normality or absence of the vestibulo-ocular reflex (VOR). The patient should be sitting upright staring at the examiner's nose. The examiner turns the head from the midline sharply to one side 30 degrees. The test is positive if the eyes make saccades to refix on the nose target. In the illustration the test to the left is normal (eyes fixed on target). Thrust of the head to the right results in corrective saccades to the left, indicating a right VOR abnormality. Image source: Canterbury District Health Board, 2013. "The Blue Book": Management Guidelines for Common Medical Conditions (15th Ed.).
Prof. Michael Halmagyi, originator of the head impulse test, demonstrating its application. Video source: Jeremy Hornibrook
The VOR abnormality can be recorded with the high frequency vHIT camera to demonstrate the head velocity with catch-up saccades as a consequence of the inadequate VOR response. Serial recordings can be used to document recovery over succeeding weeks.
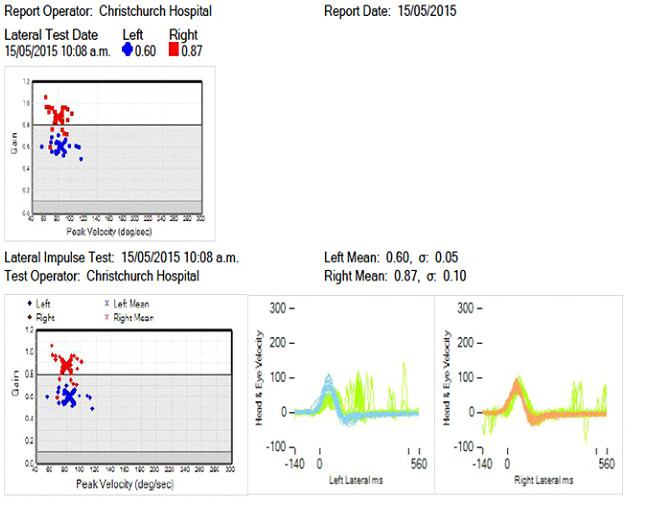
Video head impulse test (vHIT) on a seventy year-old male with recent left vestibular neuritis. With a head impulse to the right the eye velocity(green) follows the head velocity (brown). With a head impulse to the left the head response (blue) is followed by an impaired vestibular eye response with subsequent abnormal "catch-up" saccades (green). The computer calculates the VOR "gain" (eye velocity relative to head velocity) which is below normal on the left side.
Management
Initial management is with vestibular/nausea suppressant drugs (prochlorperazine,cyclizine, ondansetron) and early mobilization. There is some evidence that corticosteroids lessen the vestibular deficit. After the acute phase faster of recovery of balance is achieved if the patient is instructed to perform daily VOR head excercises, often demonstrated and reinforced by a vestibular physiotherapist (See Balance Rehabilitation).
About 60% of patients achieve full vestibular nerve recovery in about 10 weeks, as measured by objective recordings of the VOR. However clinical recovery occurs much earlier through adaptation mechanisms in the central nervous system. Even in those who do there is not a clear relationship between their VOR gain (eye relative to head velocity) to their symptoms, suggesting that central nervous system and personality factors may be operative. A small proportion of patients are left with residual symptoms.
"Recovered" vestibular neuritis patients can sometimes develop anxiety about their balance. This can progress to a condition known as perpetual perceptive and postural dizziness (PPPD).
- Assoc. Prof. Cynthia Darlington